When UNC's Doctors Go Dark
The Post-STEMI Cover-up, and the Four Calls That Exposed It
Syndicate File: 005
Context for New Readers
If you’re new to this series, Syndicate File: 004 revealed how John Boger — a Navy veteran and a world-class diesel mechanic — was sent home from UNC Hospital just two days after a widowmaker STEMI heart attack, only to be ordered back to work five days later.
The doctor who signed that return-to-work order had never examined him.
The cardiology team ghosted him.
And the nurses who tried to raise concerns were left unanswered by the very physicians they called.
What no one realized at the time was that the discharge wasn’t just negligent. It was retaliatory.
Why?
Because John’s wife had pushed back — and pushed back hard — against an inexcusable affront to her husband.
She had challenged a second-year cardiology fellow for falsely labeling John a heroin user.
She had confronted that same physician’s discomfort with treating a man who arrived covered in grease, sweat, and the reality of hard labor.
And by speaking the truth about that mistreatment, she triggered the one thing these institutions can’t tolerate:
Exposure.
All they ever wanted was basic standard of care. Not special favors. Not lawsuits.
Just what anyone should expect after surviving cardiac arrest:
A safe discharge. A chance to recover.
And they should’ve gotten it — because the stent worked.
John’s artery was reopened.
He should’ve been on the path to recovery.
Instead, it became a moment he was set up to fail.
In response, the task of writing John’s return-to-work order was delegated to an Internal Medicine resident who had never laid eyes on him.
That order was handed over with no care coordination, no discharge planner, no ICU nurse — none of the usual steps that signal continuity of care.
Instead, the entire discharge was overseen by the cardiology fellow — just 48 hours after John’s cardiac arrest.
Then he was pointed toward the doors of the ICU and told to leave.
There was no wheelchair.
There was no escort.Just: Get up. Walk out. Go.
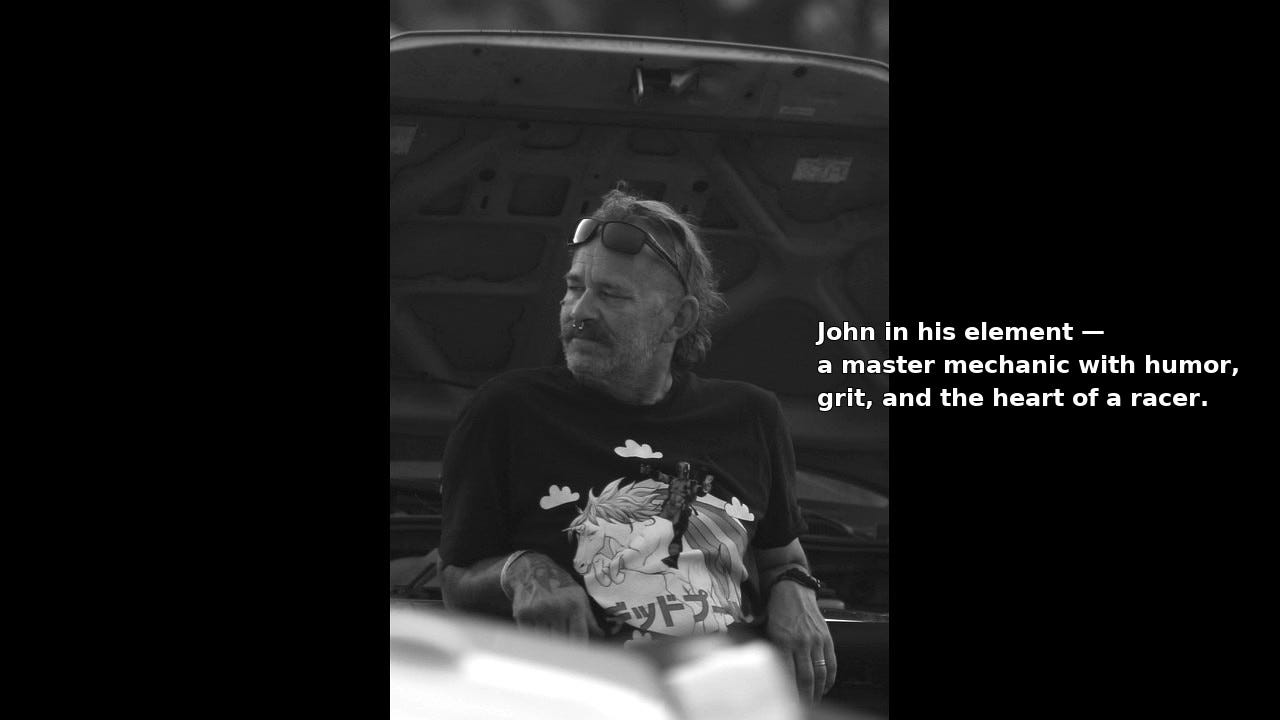
He was a man built for work.
John had spent his life, his mind, and his body doing the kind of work most people can’t — precision diesel, manual lifting, and performance engineering. He loved it, and he was built for it. But the pandemic changed everything. The stress of supply chain instability hit hard. At one point, parts for basic repairs were impossible to get, and even a day’s worth of job tickets wasn’t guaranteed.
He had already gone through two full cardiac workups back in 2019 — both completely clean — when the real culprit turned out to be a misdiagnosed gallbladder infection. But by 2024, the stress had built up, and it finally hit his heart.
He survived that heart attack.
What he didn’t survive was the system’s response.
He needed just a few weeks off to recover.
They couldn’t even offer him a wheelchair.

What followed was sixteen months of institutional retaliation:
Medical abandonment
Coordinated smear campaigns
Financial sabotage
Legal obstruction
Not just from UNC, but from Duke Health, State Employees’ Credit Union (SECU), national insurance carriers, law enforcement, a convicted felon currently on active Federal probation, and even the North Carolina court system.
All of this could have been fixed with a simple correction and a sincere apology.
Instead, it triggered a multi-institutional response so wildly disproportionate it bordered on the absurd.
Two hospital empires
A state-chartered credit union
A national insurance carrier
And the judicial system
All mobilized against one disabled man and his family.
Not because they were dangerous.
But because they had the evidence — and they wouldn’t let it go.
They didn’t treat him like a patient.
They treated him like a problem that needed to disappear.
Maybe you think this couldn’t happen to you.
But all it took was one woman asking:
“Why would you write that?”
And the weight of billion-dollar institutions came crashing down on her family.
This is no longer just a malpractice story.
It’s a case study in how powerful institutions close ranks — across medicine, finance, insurance, and the judiciary — when even a single vulnerable family threatens to expose their complicity.
And it all started here.
This installment picks up just days after that retaliatory discharge, when John and Kimberly begin calling every number they can find to ask:
Who signed that order?
Why did this happen?
And why did everyone vanish when we started asking questions?
When Doctors Go Dark
What happens when doctors vanish — not because they don’t know what to do, but because Risk Management is figuring out how to spin or suppress a blatant reckless deviation from standard of care?
Nurses — who don’t have decision-making authority,
Are left fielding patient questions,
Contradicting unsafe orders,
Giving advice outside their license,
And trying to hold the line medically, ethically, and emotionally, with zero institutional backup.
That’s what happened here.
By the time John Boger was discharged from UNC Hospital — just 48 hours after a massive STEMI, cardiac arrest, cardiogenic shock, and two stents placed in the artery that feeds the heart’s primary pump — he was ordered back to work.
Not recover. Not rest. Work.
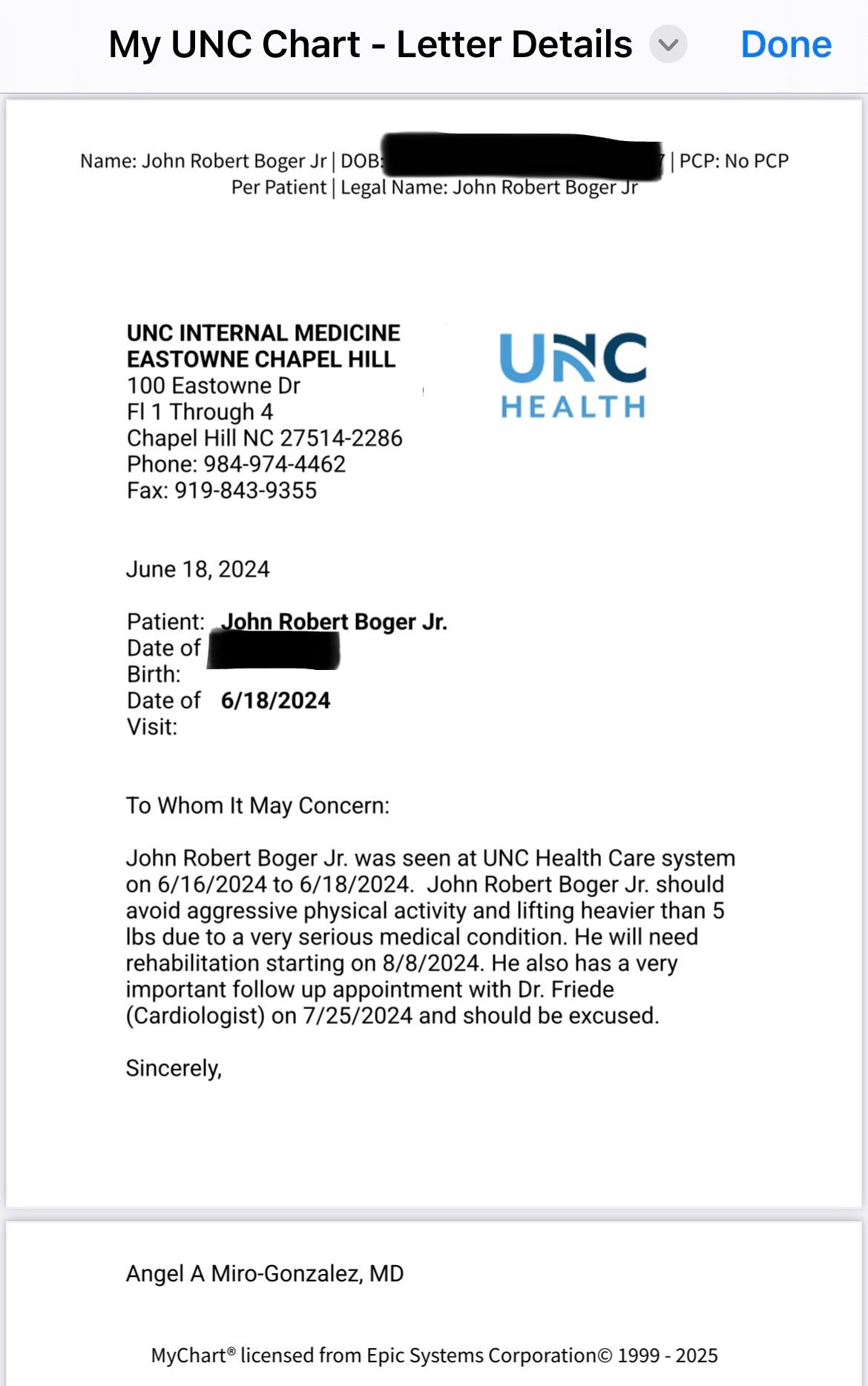
The discharge was overseen by Dr. MaryKate Carrillo, a second-year cardiology fellow. And the return-to-work order? That was signed by Angel Miro-Gonzalez , a second-year internal medicine resident who had never examined John, never laid eyes on him except perhaps as an observer in the cardiac cath lab.
They sent him back to work as a Ford Senior Master Diesel Technician — a job that meant crawling under truck chassis, torquing suspension bolts with 20-pound wrenches, and slinging 150-pound tires all day long. The next week was forecast to be the hottest in North Carolina in over a century — and his shop wasn’t even climate controlled.
He was still having chest pain. Still dizzy when standing. Still out of breath walking to the mailbox. And they were sending him into a heat wave to lift truck tires.
As reported in Syndicate File: 004, it took several days after returning home from his heart attack for John to begin grasping what had actually happened at UNC Hospital — an experience shaped by the decisions of Dr. MaryKate Carrillo, a second-year cardiology fellow still in training. Just a short time earlier, she had been a resident herself. But on that day, she was the one directing care — and it was under her supervision that the decision was made to send John home just 48 hours post-STEMI, with no support and no plan.
By Friday, just three days after discharge, the realization began to set in: the return-to-work order — issued less than a week after a heart attack and signed by another junior doctor, Dr. Angel Miro-Gonzalez, then a second-year Internal Medicine resident — wasn’t just premature. It was reckless. Death was a possible outcome.
That same day, John and Kimberly began making phone calls for clarification. They contacted both the UNC Department of Cardiology, where Carrillo was training, and the UNC Department of Internal Medicine, where Gonzalez was still a resident. These calls would become the first domino in a chain of four explosive conversations — each one peeling back a new layer of institutional failure, and each one caught on tape.
As detailed in the previous article, the first person to respond was Nurse Holly, an Internal Medicine RN. She was clearly stunned — not just by John’s condition, but by the fact that a man so recently discharged after cardiac arrest had been told to return to work without cardiology follow-up. The recording of that call is as damning as it is heartbreaking.
Holly promised to escalate the issue internally — and made it clear she would never advise John to return to work until a real physician had reviewed the case and taken responsibility for the decision.
This Should Have Ended With an Apology
The tragedy of this story is that it never needed to become one.
The discharge that sent John Boger home — just two days after a massive heart attack — with a return-to-work order for five days later, wasn’t just reckless. It was a recoverable mistake. The kind of failure that should’ve triggered an emergency care review, a corrected plan, and a sincere apology.
Instead, UNC and later Duke, triggered a system-wide defense mechanism.
What followed wasn’t medicine.
It was escalation.
It was retaliation.
It was institutional damage control — designed to protect reputations, not patients.
Most people don’t lawyer up after nearly dying. They’re still trying to breathe. They want follow-up appointments, medications, answers — not depositions.
And even if they did want legal help, good luck finding an attorney willing to take on a major North Carolina hospital. Unless someone gets murdered in the hallway, the doors don’t open. The system is nearly immune.
John and Kimberly weren’t chasing a payout.
They were just trying to stay alive.
But when they started asking questions, every system turned against them — medicine, finance, insurance, even law enforcement.
What should have been a simple correction became a coordinated, 16-month campaign to erase the harm… and discredit the witnesses.
That’s why these phone calls matter.
They don’t just document medical confusion.
They capture the moment the lie broke containment — and the scramble by institutional gatekeepers to patch it back together.
“He Shouldn’t Be Going Back to Work.”
— Carroll, RN, Cardiology Nurse Line, June 21, 2024
What you’re about to hear is a nurse trying to steady a collapsing system.
Carroll was calling from Dr. Kevin A. Friede’s office in UNC’s Department of Cardiology, just three days after John Boger had been discharged from the ICU following a “widowmaker” heart attack. On his kitchen table sat a return-to-work order — written by a second-year resident who had never even spoken to him. It sent him back to one of the most physically punishing jobs in the trades, five days post-STEMI, no restrictions, no rehab plan, no follow-up.
Carroll wasn’t part of that decision. But she was the one left to answer for it.
Assistant Professor of Medicine
Associate Director, Interventional Cardiology Fellowship
Associate Director for Research, Cardiovascular Disease Fellowship
📄 Read the full transcript of the call
“I Don’t Suggest Going Back Yet”
One of the first things Carroll says, after confirming John’s case, is immediate and clear:
“I don’t suggest going back yet, if you’ve gotta do lifting 150 lbs, tires and that type of thing.”
She doesn’t wait for more data. She knows something is wrong. You can hear it in her voice — not panic, but unease. The kind that creeps in when a frontline clinician realizes they’re staring at the fallout of someone else’s mistake.
She asks about his job, rehab, and whether the employer will allow time off. Not bureaucratically. Compassionately. She’s already working on the problem.
“I Want to Hear from Dr. Friede First”
Over and over, Carroll defers to Dr. Friede — not because she lacks judgment, but because she knows how serious this is.
“I don’t want you to go back before I talk to Dr. Friede... I’d rather play it safe.”
This is the moment where the scale of the institutional failure becomes clear. The resident who signed the RTWO? Gone. The fellow who pushed John out the door? Unavailable. And now Carroll — a nurse with no authority over discharge — is being forced to triage a dangerous order after the fact.
So she does the only safe thing she can: she refuses to confirm the order. She becomes the first voice in the entire UNC system to say: This wasn’t right.
John wasn’t looking to argue. He just wanted a straight answer.
“Yeah, I talked to him a little bit while I was there,” he said, referring to Dr. Friede. “And I would take anything he says to heart. If he tells me I’m good to go, I’ll be good to go.”
But that answer — the real one, grounded in his condition and the brutal reality of his job — wouldn’t come until the following week. And when it did, it wouldn’t be the correction they were hoping for. It would mark the beginning of something far worse: Dr. Friede’s quiet decision to protect the hospital, the resident, and the discharging fellow — at John’s expense.
What should have been a moment of trust became the opening move in a cover-up.
And it would cost John everything: his career, his heart, and the security of the family who depended on him.
Carroll becomes the first voice in the entire UNC system to say out loud what everyone else had avoided:
This wasn’t right.
“Oh, Mmmmm…” — When Carrillo’s Name Comes Up
John explains that the discharging fellow, Dr. MaryKate Carrillo, had been told exactly what kind of work he did — the heavy labor, the hour-long commute, the danger of going back too soon. Her reply, he says, was: “Oh, you’ll be fine.”
Carroll pauses.
“Oh. Mmmmm.”
It’s one of the most revealing moments in the call. A nurse hears a colleague’s name — and immediately knows something went sideways. That single syllable says what the chart never will.
“Don’tcha Dare Do That”
The call ends with Carroll doing what no doctor had yet done: speaking to John as a human being.
“Don’t say, ‘I’m already at work, I’ve got to push through the day.’ Don’tcha dare do that.”
It’s not protocol. It’s protection. A last-minute catch before a bad order turns into a body bag.
Carroll promises to follow up once she speaks to Dr. Friede. She doesn’t gaslight. She doesn’t deflect. She tells the truth she can see, and she buys him time.
This is the first moment the system stutters. The first time someone on the inside quietly signals:
“We know something’s wrong.”
Carroll didn’t fix the system. But she was the first to admit it had failed.
“That Just Really Bothers Me.”
— Nurse Holly, Internal Medicine, June 21, 2024
Nurse Holly wasn’t supposed to be part of this story.
She was supposed to be the exception.
The one who called back.
The one who laughed with John, told him to take it easy, sympathized with the botched discharge, and promised to follow up the next week.
“That just really bothers me,” she said after hearing what happened to him at UNC.
And she meant it.
But what makes Holly’s call so important — and so gutting in retrospect — is what it reveals underneath:
Even those who care get silenced.
“That’s What I Was Going to Say Too.”
John tells Holly that a cardiology nurse — Carroll — had just told him not to return to work yet. Not without a full re-evaluation. Not without a new clearance letter from Dr. Friede himself.
“She wants to talk with him and get him to write his own note before I go back to work,” he says.
“That’s what I was going to say too,” Holly replies, with relief.
This isn’t two departments coordinating care.
It’s two nurses, independently, trying to undo a mistake that should never have happened.
“I know I don’t have a horse in this race,” Holly adds, “but with what you’ve had going on... it’s probably a good idea, with the type of work you do.”
She’s speaking outside her license.
Just like Carroll, she’s stepping in because the doctors vanished.
And just like Carroll, she’s about to disappear.
“Everybody Said It Was a Bad Idea. Except Her.”
John tells Holly the truth: every single person he’s spoken to — his wife, his employer, other staff — agrees that going back to work so soon is dangerous.
“Everybody I’ve talked to said it’s not a good idea,” he says, “except for that Dr. Carrillo who wants me to go back to work.”
Holly doesn’t defend Carrillo.
She doesn’t sugarcoat it.
She sides with the patient.
“No… well, we’re gonna see what we can do to fix this up.”
She tells John she used to work cardiac stress testing and cath recovery.
She knows what happens to bodies like his under strain.
She knows the risk. And she knows what’s missing: follow-up, rest, cardiology oversight.
For just a few minutes, Holly believes they can stop the spiral.
She was wrong.
“I May Touch Base With You Next Week…”
Holly doesn’t just answer the phone. She steps in.
“I may just touch base with you next week to see how you’re doing. Is that alright?”
She’s not required to follow up.
This isn’t protocol.
It’s instinct.
The kind of instinct that gets you written up.
Because what happens next proves she was likely told to stop.
The following Monday, John is summoned to Dr. Thomas Keyserling’s clinic — an appointment that will be covered in the next installment. The tone there is hostile. The nurse who greets him is openly suspicious. She references Nurse Holly by name, with visible disdain, as if caring too much had crossed some invisible line.
From that moment on, Holly is gone.
No callback.
No follow-up.
No contact of any kind.
Not because she didn’t mean to.
But because someone made sure she couldn’t.
This Wasn’t Just a Weekend Crisis. It Was the Beginning.
At one point in the call, John tries to laugh off his stress:
“Yeah, stressing out a little bit about having to go back to work didn’t really help the situation either.”
“No, it doesn’t,” Holly says. “I know.”
She acknowledges that cardiology hasn’t scheduled a follow-up until late July — more than a month away — and says plainly:
“I don’t like that either... especially them going to send you back [to work].”
Holly knows the truth:
STEMI patients are high-risk in the weeks after discharge.
This man is still short of breath. Still dizzy. Still recovering.
He needs rest — not pressure.
And she knows what it looks like when protocol has broken down.
She saw it.
She tried to stop it.
And then. she was vanished.
“What Was Your Name Again?”
— John Boger, 10 minutes into a Saturday call from UNC Internal Medicine, June 22, 2024
📄 Click here to read the full transcript
Note: This is one of only two calls in the series where only one side of the conversation was captured. The original phone used to record has since been lost due to device failure. The sequence presented reflects the best available recollection, but the exact order of this and the Miro-Gonzalez call cannot be confirmed.
It’s a Saturday. No office hours. No scheduled appointments. No open clinics.
And yet, John Boger gets a call — not from Cardiology, where he was hospitalized just days earlier after a “widowmaker” heart attack. Not from Dr. Kevin Friede, the attending who oversaw the ICU admission and signed the discharge. Not from Dr. MaryKate Carrillo, the cardiology fellow who coordinated the exit and authorized the return-to-work order. And not from Dr. Angel Miro-Gonzalez, the Internal Medicine resident who signed that order without ever examining the patient.
The voice on the other end is someone John has never met.
Dr. Thomas C. Keyserling, from Internal Medicine. He won’t even say his name until the end of the call — and John will have to ask for it.
A Call from the Inside
Keyserling isn’t calling from a personal line. He’s calling from a hospital landline inside UNC. Not from home. Not while on call. From within the building.
And he isn’t calling to check on a patient. He’s calling to manage a situation.
The long silences on the tape are telling — not because John is rambling, but because Keyserling is doing most of the talking. Calm, deliberate stretches. No medical orders. No new plan. Just quiet redirection toward a Monday clinic visit.
This isn’t care.
It’s containment.
When the Wrong Doctor Calls, It’s Not About Medicine
John didn’t have a primary care doctor at UNC.
He was a Cardiology inpatient.
Friede was his attending.
Carrillo was Friede’s fellow.
It was Carrillo who gave Miro-Gonzalez the green light to write the RTWO — despite the fact that he’d never examined John. She then handed the discharge note to John herself — a task typically performed by a nurse — and had him walk out of the ICU, anemic from blood loss, a significant hematoma in his groin, without a wheelchair, without escort.
Friede signed off on all of it.
He is the attending.
He owns the discharge.
And yet, when the fallout begins, Friede doesn’t call.
Keyserling does.
Why?
Because by Saturday morning, the internal alarms had been tripped. Two nurses — one from Cardiology, one from Internal Medicine — had flagged the order. Risk Management was now involved. And Risk needed a surrogate.
This Would Have Been Handled Differently — Once
If this had happened 15 years ago, it would’ve been fixed in a few quick calls:
“My fellow handed it off.”
“Your resident wrote it.”
“But you discharged him.”
“Fair. I’ll fix it.”
But this isn’t that era.
Today, what used to be a clinical decision gets routed through an armada of risk-averse administrators who don’t treat patients — they manage exposure. They speak in script. They stall. They work from behind badge lanyards and clipboard walls.
They don’t solve the problem.
They reframe it.
They assign surrogates.
Carrillo vanished.
Gonzalez stayed silent.
Keyserling got the call.
The Fixer Shows Up Late
Keyserling’s tone is calm and practiced. He fills the call with long-winded observations that resolve nothing. John describes dizziness, shortness of breath, and the physical stress of having to drive to his workplace to drop off the RTWO in person — and the only result is a referral to Internal Medicine for Monday.
That was the point.
This wasn’t a clinical check-in. It was a narrative redirection — shifting the case away from Cardiology, away from the nurses who flagged the danger, and into a department the hospital could control more tightly.
That Monday appointment wouldn’t bring clarity. It would bring confrontation.
The gloves would come off.
The warmth would vanish.
And Keyserling’s clinic nurse — furious that John had dared to reach out to Internal Medicine in the first place — would finish the silencing that this call began.
“Why Would You Write That?”
— Kimberly Boger, Sunday phone call with Dr. Angel Miro-Gonzalez, June 23, 2024
📄 Click here to read the full transcript
Note: This call was made to Dr. Miro-Gonzalez inside UNC’s CICU. Only John and Kimberly’s side of the conversation was recorded due to UNC’s internal VoIP or signal-blocking system. All other calls in this series preserve both sides.
By Sunday, John had already received a call from Dr. Thomas Keyserling arranging a Monday appointment to address the dangerous return-to-work order.
But John’s mind doesn’t operate on verbal reassurances. He’s a former U.S. Navy nuclear engineer — a man trained in strict systems of accountability, hierarchy, and procedural clarity. After his military service, he built diesel engine modifications so precise they shattered NHRDA world records. His entire framework is built on documentation, paper trails, and chain-of-command logic.
So when there was no formal correction to override the original return-to-work order — nothing he could hand to his boss before the Monday shift — John panicked. Not because he didn’t trust the clinic appointment, but because there was no new order. Nothing in writing. No procedural override.
And so, on Sunday afternoon, he tracked Dr. Miro-Gonzalez down in the ICU.
He needed a correction. A real one.
What he got instead nearly broke him.
A Visceral Collapse
The call begins with John calmly asking for clarification. Then he explains — in detail — that he’s short of breath, that his heart races with minimal effort, that he nearly passed out trying to drive to work. He reminds Gonzalez that he works on concrete, lifts 150-pound truck tires, and was told that a fall on blood thinners could kill him.
When Gonzalez offers no useful response, Kim tells John to ask him why he wrote the note in the first place.
He starts to ask.
And then—he breaks.
“Jesus!”
“Oh Jesus fucking Christ!”
His voice crumples under the weight of it all. As you listen to the call you immediately visualize John grabbing his chest. He’s crying out on a phone call to the very doctor who signed the order that started all this — and Kim, hearing the distress, grabs the phone from his hand.
He’s in active chest pain. He’s crying out. Coughing. Gasping.
This is what trauma sounds like when it’s recorded in real time.
This is what institutional harm sounds like through the body of a patient. It’s not just disturbing — it’s visceral.
This was a man already physically vulnerable after a massive STEMI and cardiogenic shock, now being asked to correct the institution’s mistake himself, while the doctor who signed the note offers only vague noncommittal responses.
This is what medical trauma sounds like.
Interpretive Dance
Miro-Gonzalez didn’t issue a proper correction.
He didn’t say the RTWO was an error.
He didn’t clearly document symptoms.
He didn’t restrict lifting.
He didn’t state the obvious: John had had a heart attack.
Instead, he entered a second return-to-work order — one so vague, noncommittal, and stylized that Kim later called said “It’s written like interpretive dance. A Twyla Tharp routine masquerading as clinical documentation.”
“It wasn’t a note. It was choreography.”
“He sidestepped every fact, floated around liability, and tried to make that pass as care.”
This wasn’t a clarification.
It was a cover.
It said almost nothing.
And it did even less.
A Backdated Rewrite
The new RTWO was entered into the chart after the Sunday phone call — but backdated to June 18, 2024, the day of discharge. Its tone was soft, unclear, and visibly constructed to protect the physician, not the patient.
Critically:
This note did not exist in the chart at the time of the prior calls with Nurse Holly, Nurse Carroll, or Dr. Keyserling.
If it had been there, those calls wouldn’t have happened.
No nurse would have flagged the chart.
No internal alarm would’ve sounded.
No Risk Management deployment.
No containment call.
The note was inserted after the fact — to appear as though it had always been there.
Above: The second RTWO issued by Dr. Miro-Gonzalez. The document is vague, noncommittal, written 5 days after it is dated
Backdated Chart Entry: A False RTWO Note
The second return-to-work order was entered into the UNC chart system after John’s distress call to Dr. Miro-Gonzalez on June 23, 2024 — but it was illegally backdated to June 18, 2024, the original discharge date.
This backdating gave the false appearance that the updated note had been part of the clinical discharge.
It was not.
At the time of the calls made by Nurse Holly, Nurse Carroll, and Dr. Keyserling, this note did not exist in the record.
Had it been present, none of them would have flagged the case, called Risk Management, or scheduled damage-control appointments.
This deliberate retroactive insertion of a falsified medical directive — timed to coincide with institutional containment — is a textbook example of fraudulent documentation, under both medical ethics and legal standards.
It concealed material risk, misrepresented patient care, and obstructed clinical accountability.
UNC later revoked portal access to the original record, sometime after John was admitted to Duke — further obstructing verification.
Oddly enough, only recently has his access to his own UNC electronic medical records been restored.
And Still — She Thanked Him
Kim wanted to rip his throat out.
She didn’t.
Because when you’re watching your husband collapse, you bury your rage.
You keep the fax moving.
You keep your voice even.
You play the part of the cooperative patient’s wife — because the system demands your submission before it gives you anything at all.
And so she said:
“OK. I appreciate that.”
“Yes sir. Thank you.”
Because that’s what it takes when a mistake like this detonates — and you’re still the one being asked to make it right.
It Never Stopped
This wasn’t a one-time collapse.
This was the beginning of 16 months of institutional indifference:
No treatment for panic attacks
No referral to trauma support
No cardiologist willing to document what really happened
No honest disability certification
No follow-up
No relief
And every single one of them ignored him.
Not one doctor has written that order.
Not one has told the truth.
Legal Disclaimer
All events described in this publication are based on firsthand experiences, contemporaneous documentation, audio recordings, and medical records retained by the individuals involved. The names of public-facing professionals, hospitals, and institutions appear as they relate directly to care received, publicly verifiable employment, or statements made in an official capacity.
This publication is intended as a matter of public concern and interest, and is presented for the purpose of education, advocacy, and institutional accountability. Opinions expressed herein reflect the documented understanding, interpretation, and lived experience of the authors.
Where statements suggest conclusions about intent, knowledge, or systemic patterns, they are based on clear inferences drawn from available evidence and are protected as fair comment and opinion under the First Amendment.
No part of this publication should be interpreted as medical advice.
━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━
📂 SYNDICATE FILE: 006
“The Fixer Arrives — and the Silencing Begins.”
He wasn’t the cardiologist.
He wasn’t on the discharge.
He wasn’t even supposed to be involved.
But when two nurses flagged the reckless return-to-work order that could’ve killed John Boger, UNC Risk Management sent someone else entirely.
Dr. Thomas Keyserling — a man John had never met — calls out of nowhere on a Saturday. No ID, no plan, no documentation. Just calm, quiet tones. Rehearsed detachment. A Monday appointment.
By the time John walks into Keyserling’s clinic, the cover-up is already underway.
And the tone has shifted — from polite concern to cold hostility.
The nurse scolds them for even contacting Internal Medicine.
The chart is missing critical orders.
And no one — no one — wants to admit what’s gone wrong.
This was the moment the system stopped pretending to care.
This was when the mask dropped.
🧾 Includes new transcript evidence and recording.
Coming Soon.
Only on Syndicate of Harm.
━━━━━━━━━━━━━━━━━━━
How You Can Personally Join the Fight
Helping them isn’t charity — it’s resistance.
If you’ve ever watched someone you love get chewed up by a hospital, a bank, or a court that no longer serves justice, you already know what’s at stake.
Standing with John and Kim is standing up for everyone who’s been silenced, gaslit, or ground down for asking the system to do the right thing.
John and Kimberly Boger didn’t just survive a cardiac event.
They’ve survived 16 months of coordinated institutional retaliation — from hospital systems, financial entities, and even law enforcement. Their effort to seek accountability has cost them more than most people could bear.
They’ve been:
Blocked from SSDI by doctors who refused to certify clinical disability
Obstructed from Medicaid and food stamps
Stonewalled for nine months while trying to access John’s own retirement funds
Forced to fight false criminal allegations, file protective orders, and engage in legal defense
Denied follow-up care, medication access, and clinical support
Stripped of a 35-year automotive career — including over a decade as a Ford Certified Senior Master Technician — the family’s sole source of income. That career was ended through medical sabotage, misclassification, and abandonment in violation of cardiac safety protocols
In the meantime — and only thanks to the generosity of their many friends — the Bogers have managed to weather this hurricane from hell.
Friends have stepped up to:
Furnish propane for the winter
Cover portions of the mortgage
Pay for certified mailings, court filings, and other urgent needs
But pockets only go so deep.
And a year and a half is a long time.
If not for the people who love them, who believe in their fight, and who understand what this really is — they wouldn’t still be standing today.
And all of this has come at a personal cost:
Thousands of dollars in printing, certified mailings, and federal filings
Hours in courthouse queues filing affidavits, pro se petitions, and evidence packets
Days spent recording, documenting, and preparing materials to protect not just themselves — but you
Sixteen months of sleepless nights, panic, fear, and sustained anxiety
This isn’t just about surviving.
This is about fighting back. This is about accountability.
If you’re reading this and thinking, “This could be me, or my spouse, or my parents” — that’s the point.
This isn’t a handout.
It’s an act of resistance.
It’s standing in solidarity against institutional malfeasance and protectionism — placed above the value of human life.
Your support helps keep this public. Independent. Undeniable.
The family has already done the work.
Now they need a way to keep going.
If you believe in exposing this — help us finish it.
🧭 Support Their Fight to Finish What Was Started:
👉 GiveSendGo | Support John Boger’s Fight for Medical Safety