"Oh Jesus!" The Nurse's Reaction at UNC Hospital (Recording Released)
First recording in the Boger Case. Institutions Implicated. More to follow.
Syndicate File: 004
“Oh Jesus!” — The Nurse’s Reaction to the Truth at UNC (Recording Released)
I owe readers an explanation for my silence on the case of John and Kimberly Boger. The pause wasn’t to step back — it was to gather more evidence. And they’ve provided plenty. Evidence so extensive, so damning, that it defies ordinary comprehension.
What began as something small has revealed itself as a chilling pattern of patient abuse and institutional betrayal — a story that will unsettle anyone who encounters it.
The torment and the fight isn’t over. It’s still ongoing.
The scope of this story has expanded far beyond anything the Bogers could have imagined. It grew so vast that recounting every development became nearly impossible — culminating in Kimberly’s unlawful detainment, which crossed into false-arrest territory on August 26, 2025, as she tried to finalize the rollover of her husband’s retirement account.
Yes — it has gone that far.
The institutions caught on tape span the full ecosystem of failure:
Hospital and university executives
Healthcare staff
Credit union officers
State and municipal employees
Court and law enforcement officers
And other actors involved in what one can only deduce as a sixteen-month institutionally coordinated campaign
Some of what you’ll hear will shock you. Others will simply confirm what many already suspect. But all of it will echo the moment one nurse hears the truth and breathes:
“Oh Jesus!”
The actions taken by individuals across multiple institutions—over more than a year—to suppress, discredit, isolate, and financially devastate a disabled patient and his advocate should disturb every one of us. Their only “crime” was seeking the basic standard of care — not just what any of us would expect, but what we are theoretically guaranteed under government healthcare regulation. What they received instead was retaliation, constant scrutiny, intimidation, harassment and abandonment.
This is not merely a story of system failure. It is a story of people—of those who enforce cultures of self-preservation at any cost. In the beginning, the Bogers couldn’t imagine how far it would go. Now they know. And soon, the public will too.
There will be no more silence. There will be no more institutional internal siloing. Exposure is the only remaining recourse.
Not for spectacle, but to put them on notice—and to compel them to stop.
The Recording
I’ll cut to the chase—because what most people want is evidence.
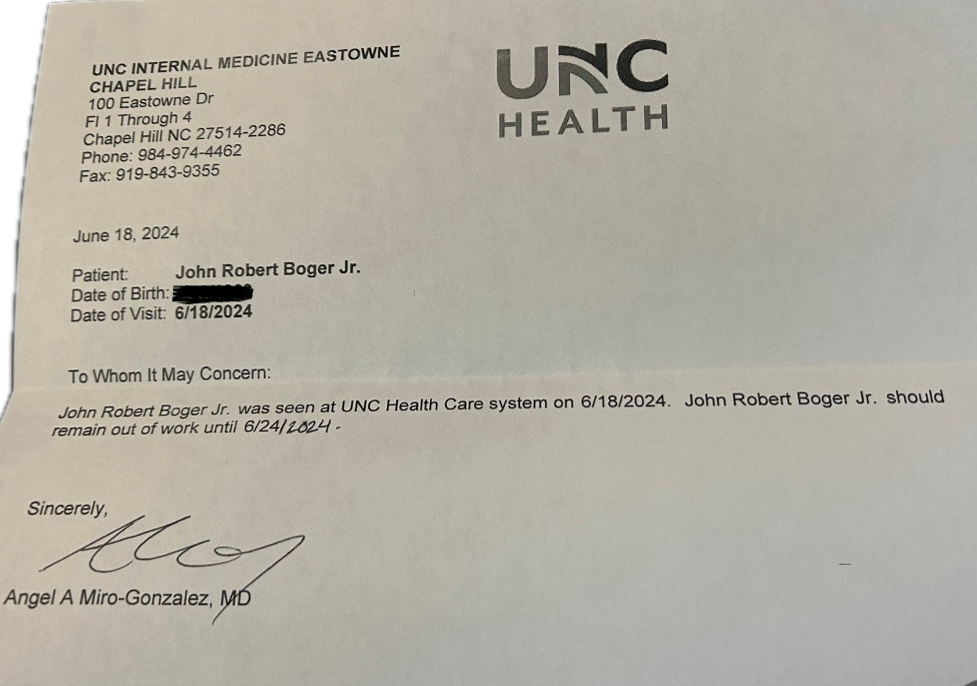
This is the recording of a desperate phone call between John and Kim Boger and a nurse in UNC Hospitals’ Internal Medicine Department. It took place on a Friday, just three days after John’s release following a “widow-maker” heart attack. He’d been handed a physician’s order to return to work the following Monday.
John’s job? Ford Certified Senior Master Technician.
His specialty? Diesel trucks and engines.
That means routinely hefting 150-pound truck tires and swinging 20-pound torque wrenches—work that demands the strength of an ox.
By the second day at home, with the shock of the heart attack beginning to fade, John and Kim realized something was terribly wrong. Everything about his hospital stay and discharge felt off. A little research confirmed it: the required healthcare rules and guidelines hadn’t been followed.
No one—not even a desk worker—returns to a job a week after any heart attack. Hospitals are required to follow Medicare guidelines, along with additional standards from the American Heart Association or American College of Cardiology, to ensure post-MI rest, rehabilitation, and re-evaluation before any return-to-work order.
What John was handed wasn’t just reckless for his health—it was a liability for UNC Hospital itself.
This call was meant to clarify those orders. The nurse, as you’ll hear, is shocked and alarmed by what she sees in his chart.
Your first jolt comes around 1 minute 30 seconds into the recording—but don’t stop there. The full conversation is revealing from start to finish.
For readers who prefer text, the full transcribed PDF is linked below.
Read the Full Transcript link: FIRST CONTACT: NURSE HOLLY, JUNE 21, 2024
This was the first—and last—health-care professional who showed genuine sincerity toward the Bogers. Nurse Holly truly seemed to care about protecting her patient, and about calming, consoling, and reassuring his wife that everything would be all right.
If only she had known what this man and his family were about to be dragged into.
The Beginning of the Nightmare
Father’s Day – June 16, 2024
John Boger was in his shop at home in rural North Carolina, working on his Mazda Miata for the next local car rally. Among the Miata crowd and the diesel-racing community, John is an icon — known nationwide as the man who, in 2008, designed and built the World Beater Ford F-250 that broke the NHRDA world-speed record for Rudy’s Diesel Performance — the banner that truck ran under.
In the early days of that business, it was just John and the owner in a two-bay garage: one turning wrenches, the other selling parts on eBay and out the front door. Years later, John became a Ford Senior Master Technician, certified in diesel, gasoline, all-electric, and hybrid systems — the highest level of certification Ford grants.
That Father’s Day, he suffered what’s known as a “widow-maker” — a ST-elevation myocardial infarction (STEMI). Against the odds, he survived, and his early cardiac tests were remarkable. His post-STEMI echocardiogram showed such strong function that a near-full recovery — and eventual return to work after adequate rest and cardiac rehab — should have been expected.
Instead, John Boger is now 100 percent permanently disabled.
This is the story we are going to chronicle for the public — so that it never happens to another patient, another family, or another advocate again.
There comes a point in every case when the story begins telling itself. Not because it’s finished, but because the silence around it has been broken so thoroughly that denial becomes untenable. This is that moment.
The Three Percent Man
On June 16, 2024, John Boger was rushed by ambulance from his home garage to UNC Hospital in the throes of a massive STEMI heart attack. He was greasy, sweaty—yet still the picture of strength—not from gym hours, but from years spent building world-class performance engines and repairing the passenger cars that keep the rest of us safe on the road.
He was alert when he arrived at UNC. Sometime after crossing that threshold, his condition worsened. He went into cardiac arrest, was resuscitated, and placed on an intra-aortic balloon pump for post-STEMI support.
He should have been transferred to a cardiac step-down unit.
He should have had a case manager to coordinate follow-up care.
He should have been reassessed after the trauma.
48 Hours to Disaster
From the moment John crossed the hospital threshold, the clock was already ticking. Within forty-eight hours—despite cardiac arrest, invasive interventions, and visible trauma—the decision was made to release him. The system never paused. It never re-evaluated. It never admitted risk. Instead, just two days later, he was pushed out the door.
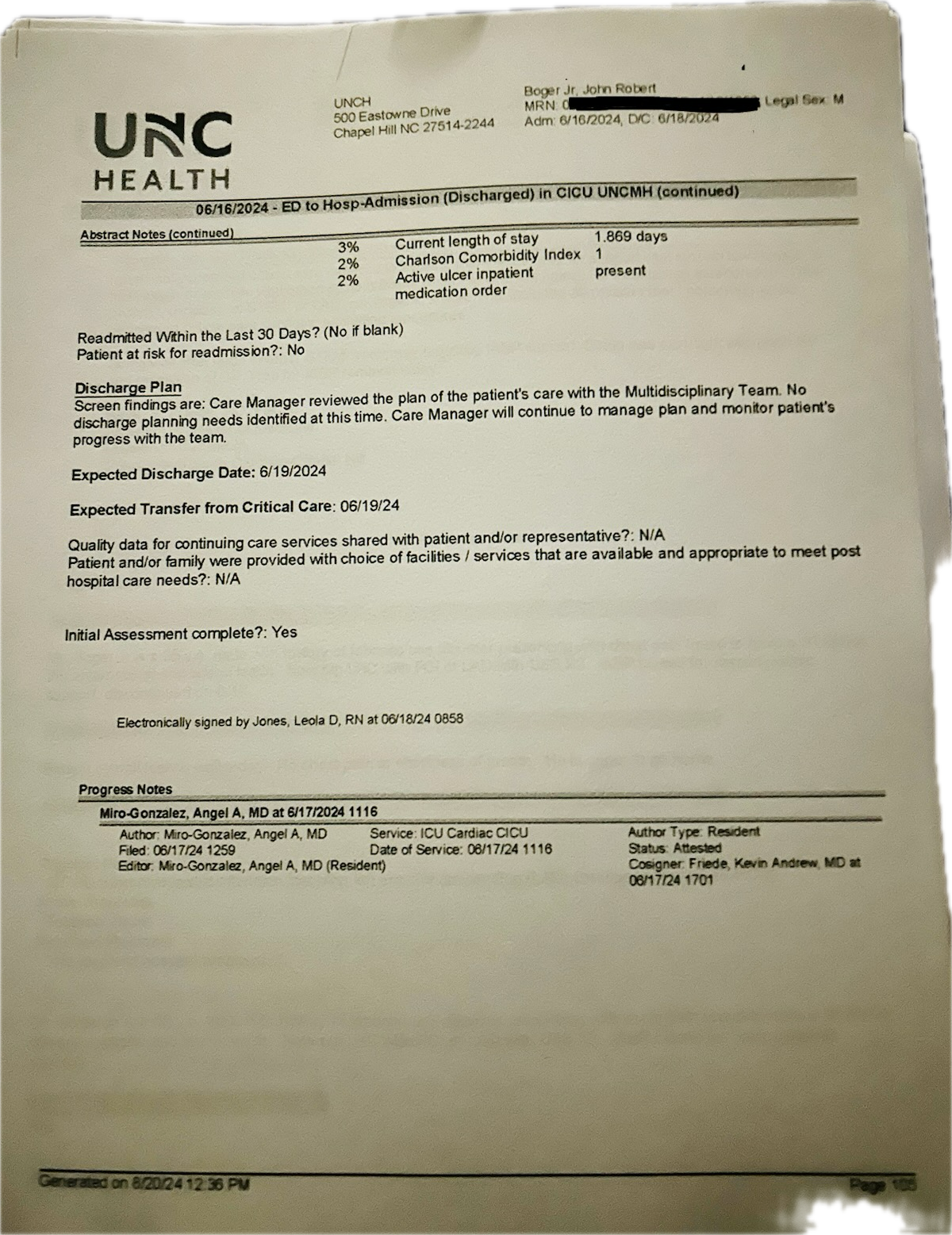
The paperwork tells a version of events designed to vanish into bureaucracy: no critical follow-ups, no needs identified, no concerns worth noting. The second day discharge-planning note written in the ICU even suggested that he would be stepped down to a lower level of care—yet that never happened. He was sent home that same day, barely forty-eight hours after lying on a table in the cath lab with his heart stopped.
Let’s be clear about what that document actually shows: it wasn’t a final discharge summary. It was preliminary.
“Care Manager will continue to manage plan and monitor patient’s progress with the team.”
Expected transfer from critical care: 6/19/24
According to that same record, his length-of-stay percentile was 3 percent—a statistic that, in EPIC’s own hospital dataset, includes patients who died during admission. In other words, John’s discharge speed placed him among the same tiny fraction of cases that either didn’t survive or were released at extreme medical risk.
Even more telling, the record states that the patient was “not at risk for readmission.” In reality, he was readmitted not once, but three times within twenty-one days of his heart attack. Each of those readmissions should have automatically triggered multiple Centers for Medicare & Medicaid Services (CMS)-mandated reviews and care-coordination protocols.
None of that ever happened.
What followed was a sixteen-month chain of EMTALA violations — a continuing failure to provide medical screening, stabilization, and coordinated transfer obligations that federal law requires of every hospital receiving Medicare funds. Each subsequent admission and discharge repeated the same pattern of abandonment, concealment, and record falsification.
This pattern of conduct demonstrates more than negligence. It reveals both the mens rea—the knowing disregard for required safety protocols—and the actus reus—the deliberate act of premature discharge that placed the patient in harm’s way. Together, they form a clear picture of willful institutional misconduct.
The Paper Trail Begins
This was no recovery. He was shoved out of the ICU by dinner time that same day.
What the document shows is not a bureaucratic glitch or a faceless system failure — it reads like a retaliatory discharge, one that prioritized institutional optics over patient safety.
It wasn’t procedural. It was personal.
The Insult
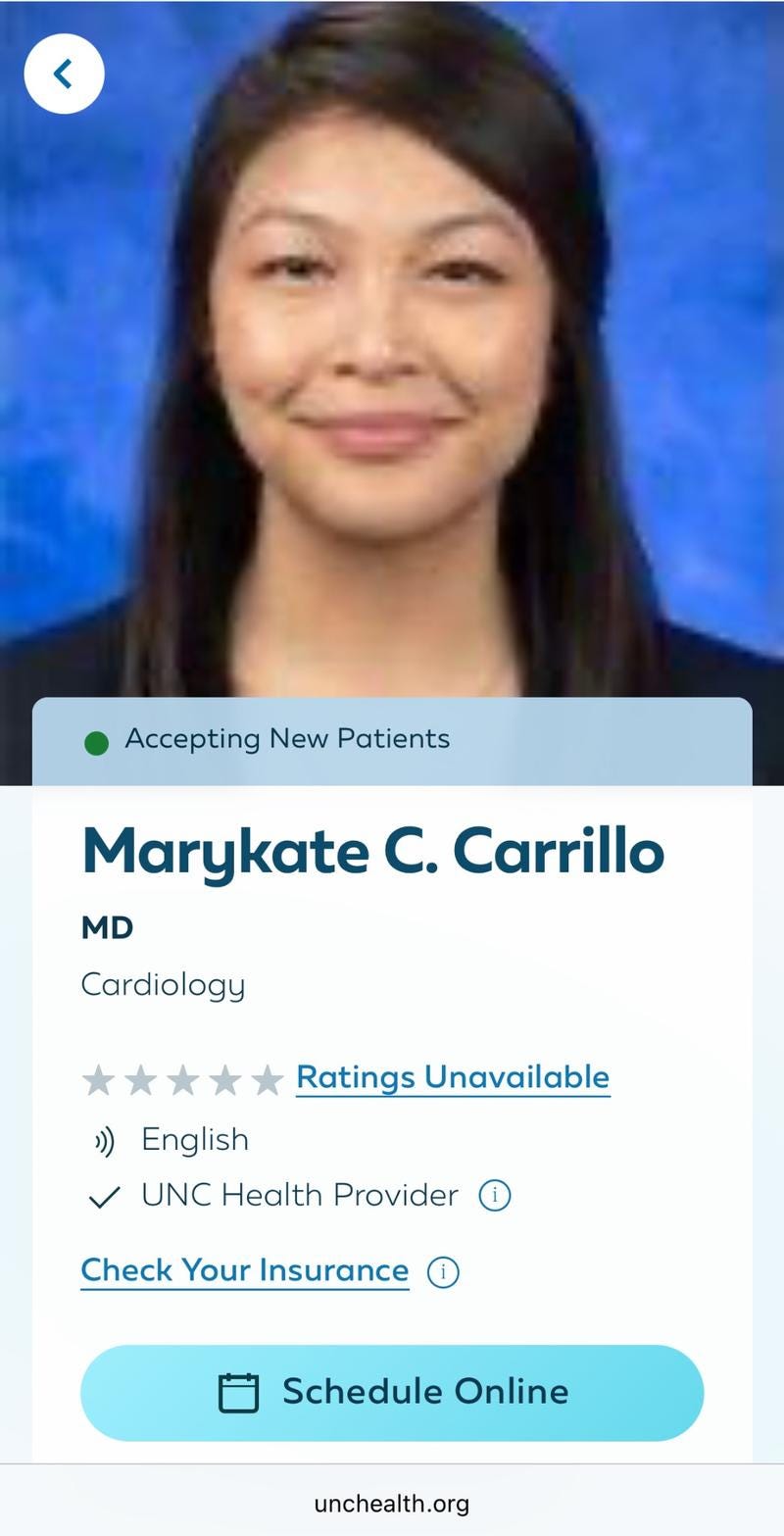
Dr. Marykate Carrillo, then a second-year cardiac fellow, entered John’s room to review his medications. Glancing at the list, she said:
“Mr. Boger, I don’t see heroin on your home medication list.”
John lay flat on his back, recovering from a STEMI and still tethered to a balloon pump inserted through his groin to stabilize his stunned heart. He wasn’t on opiates. He’d refused them because he’d had adverse reactions to them after prior surgeries. He’d never used recreational drugs of any kind. The only things he took regularly were glucosamine and chondroitin.
“Because of his joint health,” Kimberly would later say.
“You know — just like every heroin junkie prioritizes joint support.”
The comment wasn’t a medical inquiry; it was a character attack so shocking that his ICU nurse expressed shock and disbelief. Carrillo’s disdain was visible. She didn’t see him for who he was, all she saw was a tattooed man with grease-stained hands and a nasal piercing—not the kind of patient she respected.
He held no value in her world.
The Procedure
Later that same day, Carrillo was responsible for removing the intra-aortic balloon pump. She didn’t want to do it. She told the nurse:
“I really don’t want to touch him.”
The nurse refused — because nurses don’t remove IABPs. So Carrillo did it herself. Poorly. The pressure she applied was intermittent and insufficient. John developed a large hematoma and significant blood loss.
The attending cardiologist later noted that John was anemic to the point that a transfusion might be needed. Post-STEMI anemia places enormous strain on cardiac function and oxygen demand — and increases the risk of complications or death.
And yet, instead of being transferred to the stepdown unit as planned, John was discharged directly from the ICU the next day.
The hematoma was never evaluated. No ultrasound. No imaging. No consult.
Kimberly told John’s nurse they wanted Carrillo off the case. Her comments were beyond offensive. Her technique was careless. Her attitude made it clear she had no respect for the patient or the family.
Her conduct was inexcusable.
UNC left her in charge. That’s how bad it was.
The Discharge
The next day, there she was again — fully suited in surgical garb. Her face was masked, inappropriately, as if they wouldn’t recognize her. She showed no visible remorse. There was no second opinion. No conversation. Just her and someone from pharmacy, handing over discharge paperwork like a transaction.
No follow-up appointments pre-scheduled.
No driving instructions.
No lifting restrictions.
No escort.
No wheelchair.
The ICU doors opened. They were told to go.
Anyone who’s ever been in the hospital or had a loved one admitted knows that just isn’t done. It’s universally known that when you leave the hospital, whomever is accompanying you home, fetches the car and has it waiting at the lobby. The patient is more than 9 times out of 10 brought out in a wheelchair unless the patient is fully ambulatory and declines being wheeled out. Even then the nurse still has to escort the patient to the exit, observe them safely get into the vehicle, watch them drive off and then chart this event for the record.
Instead, they opened up the ICU doors and said you can go now, like a prisoner being released onto the street.
John and Kimberly had to walk blocks back to the parking garage. John did so, because he believed he was capable of doing so. Why? They told him to go. For a man like him, if they told him to, in his mind he must put forth the effort to do what he was told and that was to leave under his own power. So, he slowly, painfully and short of breath with Kimberly’s help made his way back to where she had parked the car.
When Kimberly later described this discharge:
They released him into the wild like an animal. Dogs get treated better at a vet.
What they did that day wasn’t careless paperwork.
It was a decision that had been made — and carried out — without empathy, oversight, or care.
And it nearly killed him.
What They Were Handed
They were handed a plastic bag full of medications — many of which they had never seen before. Someone from pharmacy explained what each drug was for, but no one warned them about the printed warnings on the bottles. Carrillo didn’t review them either, and no one involved in discharge stopped to consider what these medications meant for a man being told to return to work.
At the time, still in shock and just trying to leave the hospital, they didn’t question it. It wasn’t until they got home and started reading the labels that they realized what they’d been given.
Several bottles were clearly marked:
🚫 “Do not drive or operate heavy machinery.”
🚫 “May cause dizziness or fainting.”
🚫 “Take with caution until stabilized.”
No one had flagged these risks. No one asked if John had a ride home — or how he planned to get to work.
These weren’t mild meds. These were post-STEMI cardiac drugs known to cause hypotension, dizziness, syncope, and disorientation — especially during the first few days after starting them.
That part? Skipped. Glossed over. Because in these academic hospitals, everything is a team — post-MI team, discharge team, pharmacy team — and these teams follow patterns. They’ve done this hundreds of times.
But this time wasn’t like all the others.
This time, someone had shoved a man out the ICU door and told him to report back to a job slinging truck tires and torque wrenches.
The pharmacy tech likely didn’t see the return-to-work order. Why would he? It’s not routine for the pharmacy to look at those. He probably assumed, like everyone else, that the system was working — that no one would discharge a man straight from the ICU with no restrictions. That order was buried in the stack of papers Carrillo handed them.
He believed, like everyone else, that John would be resting. That he’d be seeing a cardiologist within a week or two, the way patients are supposed to.
But Kimberly couldn’t get him in for five weeks. Not without a care coordinator expediting those appointments prior to discharge.
That gap wasn’t just an inconvenience. It was dangerous.
And it started showing.
John got dizzy trying to walk.
He got lightheaded trying to stand.
Then came the day he tried to do what he was told:
Get in the car. Drive the hour to work. Deliver the return-to-work note.
And halfway there, he started asking himself if he’d even make it back.
That’s how bad it was.
And still — no one warned them.
No one stopped it.
No one even seemed to know what they’d done.
The Realization
What followed was silence. Not just from the hospital but in the house.
They were still in shock. Kimberly had watched her husband almost die. She had seen the cruelty, the indifference. They both needed time just to breathe, get their bearings and process what all had just happened to their lives in the span of three days.
It wasn’t until a couple of days later, while gathering paperwork and trying to make sense of what had just happened that the fog began to lift. At first Kimberly had been saddled with the tasks of calling for appointments with a cardiologist and Cardiac Rehab. They hadn’t even assigned him a cardiologist! She was told she had to make the appointments herself. In reality this is the job done by a Nurse Care Coordinator/Manager. That’s their primary purpose to arrange a safe discharge. They didn’t bother to assign a primary care doctor either. Another thing that is mandatory according to Centers for Medicare Core Measures after a M.I., the hospital is supposed to do prior to discharge. A primary care physician is supposed to be the one to coordinate all of the patient’s care. They didn’t call and expedite his Cardiac Rehab appointment so he could be evaluated for appropriateness to return to work. One doesn’t just send a post heart attack patient back to work! They must be re-evaluated and deemed fit. So, Kimberly was stuck calling these offices and services cold and begging for appointments. Cardiac Rehab ended up being put out until August 8, 2024! That’s almost 7 weeks after he was told to return work! It’s not supposed to work this way. Rehab first. Work comes after that and a reevaluation of cardiac function.
Nothing about this was right. They started researching post STEMI care and realized things were very, very wrong.
It was then that they really looked at the return-to-work order.
Five days. No restrictions.
It was surreal. It was reckless. It was intentional. It was insane.
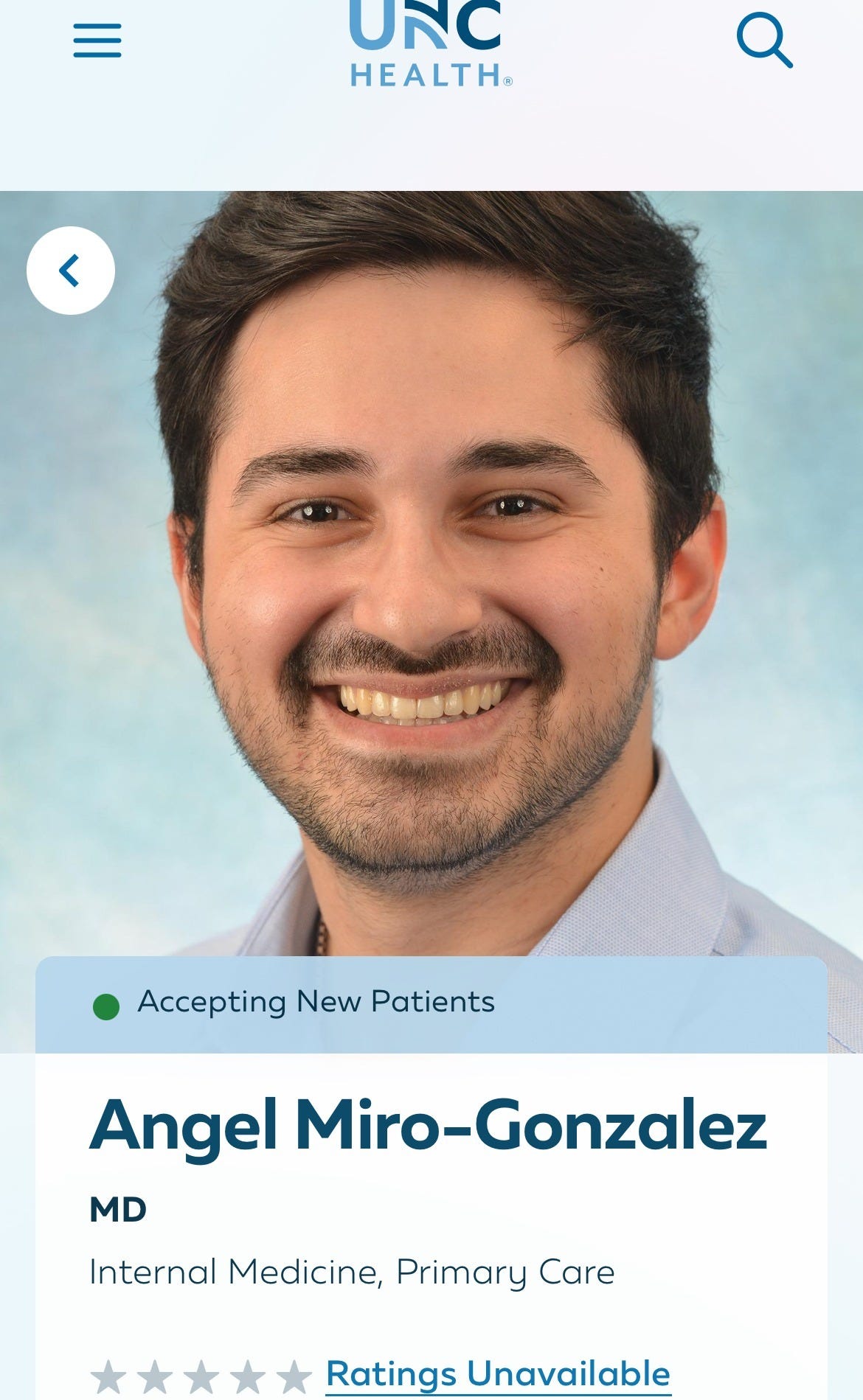
This order was signed by a second-year resident who neither John nor Kimberly ever remember seeing, Dr. Angel Miro-Gonzalez.
The Stranger’s Signature
He never walked into the hospital room.
Never laid hands on John.
Never took a history.
Never made an assessment.
He might’ve seen John wheeled into the cath lab and observed the procedure. That’s the best anyone can say. But neither John nor Kimberly recognized his face when they looked him up later — and this was the man who signed the order declaring John fit to return to work five days post-discharge.
A man recovering from a heart attack.
From cardiac arrest.
From balloon pump trauma.
From untreated anemia.
From a hematoma that he never evaluated.
And Miro-Gonzalez — a complete stranger — declared him fit to sling truck tires and operate power tools without restrictions.
He wasn’t acting as a physician.
He was a rubber stamp.
Whether he was asked to sign it or offered to do it, the result was the same:
A false document, written by someone who never saw the patient, used to justify a discharge that violated every standard of post-STEMI care.
In clinical terms, this wasn’t just poor judgment — it was false attestation under 42 CFR § 482.12 and § 482.22. Return-to-work orders are medical determinations that must be based on a direct assessment of the patient’s condition, risks, and capacity. Signing such an order without ever examining the patient — particularly one recovering from cardiac arrest, a STEMI, active anemia, and a procedural complication — may constitute fraudulent certification under both CMS guidelines and state medical board standards. It also violates the basic duty of care owed to any patient.
Not As Advertised
From UNC’s Awards & Honors page:
“UNC Hospitals was recognized for its commitment and success in implementing a higher standard of care for heart attack patients that effectively improves the survival and care of STEMI (ST Elevation Myocardial Infarction) patients.”
uncmedicalcenter.org
From UNC’s Heart & Vascular page:
“We hold a Mission: Lifeline® Gold Plus Receiving Quality Achievement Award from the American Heart Association in recognition of our fast, high-quality treatment of people experiencing severe heart attacks.”
uncmedicalcenter.org
From UNC’s news release on recognition by AHA:
“The American Heart Association presented UNC Health with multiple Achievement Awards for implementation of quality care … The Mission: Lifeline and Get With The Guidelines programs help put proven knowledge and guidelines to work on a daily basis to improve outcomes for cardiovascular patients.”
UNC Health Newsroom
While the AHA doesn’t name an exact number of days for return to work after a STEMI, their published guidance says this:
“Most people return within two to three months. This can vary based on the type of work. People with physically demanding jobs may need longer.”
heart.org
John was given five days.
John’s heart attack was a STEMI complicated by cardiac arrest. He underwent PCI with two stents placed in his left anterior descending artery (LAD) — the “widow maker.” He had an intra-aortic balloon pump, a large hematoma, active anemia, and he was never re-evaluated before being ordered back to work.
So what does the data say about return-to-work in cases like his?
Let’s start with the studies:
A cohort of 1,585 PCI patients at Aarhus University Hospital (Denmark, 2006–2008) showed that only 68% returned to work by 12 weeks, and 77% by one year.
A 2022 meta-analysis of 43 prospective studies (34,964 patients) found RTW rates of 47.3% within three months, and 80% after one year.
That same study found RTW was significantly lower for blue-collar workers (65.0%) compared to white-collar workers (81.2%), and even lower (64.1%) in jobs with elevated physical workload.
These figures reflect average conditions — patients who had time to recover.
John wasn’t given that.
He was handed a return-to-work order five days after nearly dying on a table — and sent back to a job that involved 150-pound truck tires and 20-pound torque wrenches.
In John’s case — STEMI, cardiac arrest, LAD stents, balloon support, hematoma, anemia, and a heavy-manual labor job —
These benchmarks don’t just suggest the order was premature.
They make the deviation impossible to ignore.
John was a miracle.
He came out of that hospital with a preserved ejection fraction, no neurological deficits, a resting heart rate in the 50s — numbers you’d expect from a lifelong athlete, not a man who had just flatlined.
He should have been celebrated, protected, rebuilt.
Instead, they destroyed him in the days that followed — not from disease, but from decisions.
They didn’t fail to save his life.
They failed to honor the fact that he survived.
That wasn’t just reckless.
It was categorically outside the norms for someone in his condition and profession.
This wasn’t an error. It was systemic malpractice cloaked in prestige.
To many, this doesn’t just look like malpractice.
It looks like paperwork used as a weapon.
And when they looked at each other, they knew they had to do something.
Her Name Was Holly
They began calling. Not aimlessly. But with urgency. First Cardiology. Then Internal Medicine.
Eventually, a voicemail was returned.
The nurse who called back was older. Seasoned. Cautious.
She didn’t defend what had happened. She didn’t equivocate.
She listened. And then she asked John what he did for a living.
“I’m a diesel technician.”
There wasn’t even a pause when came the words that named this entire chapter.
“Oh Jesus!”
She didn’t need a script. She didn’t need a committee. She just heard the truth.
This was the first and last healthcare professional who was actually sincere in their interaction with the Boger’s. She really seemed to care about protecting the patient and trying to calm, console and reassure his wife that everything was going to be O.K..
If only Nurse Holly had known what this man and his family were about to be thrown in to.
What This Means
This isn’t one bad interaction. This isn’t about tone or bedside manner.
This is what it looks like when someone is discharged not based on health but based on optics and exposure risk.
This is what it sounds like when another medical professional hears it all laid bare.
This is the sound of truth breaking protocol.
And it’s just the beginning.
More recordings exist. More documents will be released. And no one is going to bury this man’s story.
We told them this wasn’t just a complaint.
It’s a record.
It’s a file.
It’s an indictment.
And now you are hearing it for yourself.
This is only the beginning though!
Soon we’ll go through how, instead of reversing course and issuing a reasonable return-to-work order with a safe plan of care, this situation was escalated all to minimize the actions of Carrillo and Gonzalez.
Institution first.
Patient safety — and the protocols the public expects to protect them — went straight out the window to shield two very young doctors who had placed themselves above the patient.
They didn’t discharge him because he was stable.
They discharged him because they had judged him.
And as you’ll soon see, the institution stood behind that judgment even though they knew it could kill him.
It damned near did.
⚖️ Author’s Note
All events described in this entry are grounded in contemporaneous documentation: time-stamped medical records, direct call recordings, discharge documents, photographs, voice mails, and physical evidence preserved at the time of occurrence.
All materials were logged and retained for the purpose of legal accountability and public interest reporting.
Any opinions expressed herein are drawn from lived experience and protected commentary under the First Amendment.
🔍 Coming Soon: Syndicate File 005 — The Coverup Begins
A second Return-to-Work Order. Disappearing doctors. Whispered warnings.
UNC Risk Management retreats into Zoom rooms.
Nurses whisper warnings.
Gonzalez panics in the ICU.
And the second RTWO arrives with a digital echo they didn’t expect.
——————————————————————————————————————
Why John and Kimberly Need Your Help
John and Kimberly Boger didn’t just survive a cardiac event. They’ve survived 16 months of coordinated institutional retaliation — from hospital systems, financial entities, and even law enforcement. Their effort to seek accountability has cost them more than most people could bear.
They’ve been:
Blocked from SSDI by doctors who refused to certify clinical disability
Obstructed from Medicaid and food stamps
Stonewalled for nine months while trying to access John’s own retirement funds
Forced to fight false criminal allegations, file protective orders, and engage in legal defense
Denied follow-up care, medication access, and clinical support
Stripped of a 35-year automotive career — including over a decade as a Ford Certified Senior Master Technician — the family’s sole source of income. That career was ended through medical sabotage, misclassification, and abandonment in violation of cardiac safety protocols
In the meantime — and only thanks to the generosity of their many friends — the Bogers have managed to weather this hurricane from hell.
Friends have stepped up to furnish propane for the winter, cover portions of the mortgage, and pay for certified mailings, court filings, and other urgent needs.
But pockets only go so deep, and a year and a half is a long time.
If not for the people who love them, who believe in their fight, and who understand what this really is — they wouldn’t still be standing today.
And all of this has come at a personal cost:
Thousands of dollars in printing, certified mailings, and federal filings
Hours in courthouse queues filing affidavits, pro se petitions, and evidence packets
Days spent recording, documenting, and preparing materials to protect not just themselves — but you
Sixteen months of sleepless nights, panic, fear, and sustained anxiety
This isn’t just about surviving.
This is about fighting back. This is about accountability.
If you’re reading this and thinking, “This could be me, or my spouse, or my parents” — that’s the point.
This isn’t a handout. It’s an act of resistance.
It’s standing in solidarity against institutional malfeasance and protectionism — placed above the value of human life.
Your support helps keep this public. Independent. Undeniable.
The family has already done the work.
Now they need a way to keep going.
If you believe in exposing this — help us finish it.
🧭 Support Their Fight to Finish What Was Started:
👉 GiveSendGo | Support John Boger’s Fight for Medical Safety